Introduction
KMT2A ( MLL) fusions are relevant biomarkers in myeloid malignancies. KMT2A-PTD (also called MLL-PTD, partial tandem duplication), a non-fusion gene rearrangement, also occurs and serves as an important biomarker for Menin-inhibitors. Traditionally, KMT2A-PTDs are detected by RT-qPCR (quantitative real-time PCR). Here we report the detection of KMT2A-PTDs in whole blood samples taken from healthy donors using the Oncomine TM Myeloid Assay GX v2, which is a next-generation sequencing (NGS) based assay that enables efficient detection of multiple genetic alterations in parallel. KMT2A-PTD positive clinical research samples were used as a control in this study. This study was initiated based on reports from various healthcare professionals who observed several healthy blood donors identified with KMT2A-PTD using the Oncomine TM Myeloid Assay GX v2. As a result, we conducted tests on healthy controls and compared them with clinical research samples known to have myeloid malignancies to explore this genomic alteration further.
Methods
We sequenced 20 whole blood samples (total 104 replicates) from healthy donors at 3 different sites of Thermo Fisher Scientific TM (South San Francisco, CA; Guilford, CT; Carlsbad, CA). These whole blood samples were received from Stanford Blood Center or purchased from Discovery Life Sciences. As a control, we also sequenced 20 clinical research samples (total 85 replicates) that are known to have myeloid malignancies in both Sonora Quest Laboratories and at Thermo Fisher Scientific TM South San Francisco site. These samples were run on the Ion Torrent TM Genexus TM Software 6.6 and analyzed using the Oncomine TM Myeloid Assay GX v2 with fusion profiling, where the assay design targets 6 different KMT2A-PTD variants.
Results
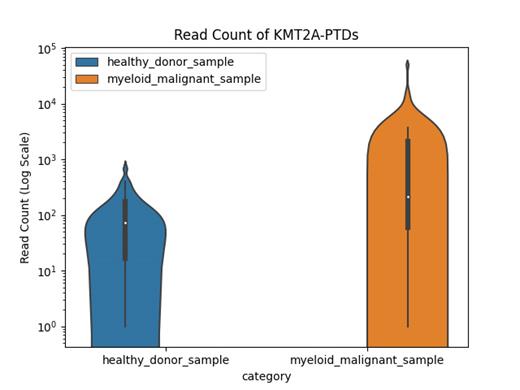
The data set has mean read length 90 - 120bp and total mapped fusion reads 20,000 - 30,000. We have found evidence of KMT2A-PTDs in confirmed positive samples from myeloid malignancies (including: AML, acute myeloid leukemia; MPN, myeloproliferative neoplasms; MDS, myelodysplastic syndromes; CML, chronic myeloid leukemia; CMML, chronic myelomonocytic leukemia; or JMML, juvenile myelomonocytic leukemia) and healthy donor samples. The read counts of PTDs detected in the healthy donor samples are on average about 1/3 of the read counts of PTDs detected in the myeloid positive samples, but the distributions overlap. Approximately 33% of myeloid positive samples have PTD read counts higher than the maximum read counts detected in any of the healthy donor samples. The sequences of KMT2A-PTDs found in both healthy donor samples and myeloid samples were further analyzed in BLAT (BLAST-Like Alignment Tool) to confirm that they match the specific exons on the KMT2A gene. Based on this data, only samples with myeloid malignancies have >2000 reads that support KMT2A-PTDs with this assay.
Conclusions
We describe the detection of KMT2A-PTDs in a range of clinical research samples, including healthy controls as well as samples with myeloid malignancies. KMT2A-PTDs were detected in healthy control samples at lower levels, however, one third of myeloid samples showed significantly higher KMT2A-PTD read counts compared to healthy controls. This intriguing finding warrants further investigation, as it opens up the possibility of conducting a prospective study to follow up on these individuals and observe if they develop myeloid malignancies. Moreover, this finding presents an opportunity for conducting retrospective studies to explore whether healthy controls previously identified with this alteration several years ago after blood donation were subsequently recorded in the health national system with myeloid malignancies.
(For research use only. Not for use in diagnostic procedures.)
Disclosures
No relevant conflicts of interest to declare.